ACUTE BACK PAIN GUIDE
How to Cope with Acute Back Pain and Promote RecoveryThe purpose of this article is to offer you some practical and usable information for coping with acute back pain and to help accelerate your recovery. The ideas and practices presented are gathered from my 25 years of working with patients suffering from back pain and sciatica.
Perhaps right now you are experiencing some of the common symptoms of acute back pain:
- A sharp, severe pain in your back
- Pain radiating down your leg
- Numbness or tingling
- Difficulty moving
- Bent or crooked posture and inability to straighten up
- Pain when you get up from a chair
- Difficulty putting on socks
- Inability to find a comfortable position or get out of bed
- Muscle spasms when you take a deep breath
Below are some tools you may find beneficial to release tension and spasms, reduce pain, restore the joy of mobility and ease of breathing and recover full function.
1. DON’T PANIC
It is normal to be afraid that something very serious is happening. Most of us in this situation think,“What if the pain doesn’t go away?” or “What if this will change the rest of my life?” Sometimes the fear of serious and permanent consequences prompts patients to decide to rush to unnecessary treatments, at times even surgery.
In a study described in the New York Times article, “Study Questions Need to Operate on Disc Injuries,” 11/22/06, data showed that no one who delayed having surgery got worse or developed permanent nerve damage. Before that study was published, patients were frequently advised to undergo surgery to “prevent a permanent nerve injury.”
Actually, in most cases, back pain, even when severe, is transient. Let go of worrying and thinking too much.
Your main job now is to get better. Everything that interferes with that must be put aside. Your attention is a high value commodity – what you focus on is extremely important.
Did you know that negative thinking could slow down your recovery? There is a “nocebo effect” (negative placebo reaction) where a person’s fear, pessimistic belief, doubtfulness and poor expectations produce harmful, injurious and undesirable consequences. Studies show that people experience the negative side effects of medications even when they received only a sugar pill. In one study, 50% became drowsy, 25% had headaches and 18% reported heaviness and fatigue.
Surround yourself with positive energy. Create your own placebo reaction or, if you are inclined to be skeptical, at least be aware of the consequences of your negative thinking. Imagine a mother lovingly caring for her crying baby. She does not assume immediately that a life-threatening disease causes her child’s discomfort. She checks the diaper, makes sure the baby is not too warm or too cold and then checks if the little one is hungry or thirsty. She tries to create a safe environment and soon enough, the baby stops crying. You, too, in a few hours or several days, can create an environment that will relieve your pain and suffering.
2. YOU ARE NOT ALONE
At this very moment there are thousands of other people in a similar situation. Back pain is very common. Statistics show that 80% of Americans will experience back pain at some point in their lives. In fact, it would be unusual for anyone to go through life without experiencing back pain at some point.
3. CONSULT YOUR DOCTOR
Your doctor will examine you to rule out any serious
illness or symptoms such as:
• Loss of bowel or bladder control (incontinence)
• Foot drop (extreme weakness or paralysis of the muscles of the leg)
• Systemic symptoms: fever, sudden weight loss, changes in general health
The doctor may recommend some tests (X-ray, CT scan or MRI) and an appropriate course of treatment including medication (for pain, inflammation or muscle relaxation).
4. LOOK FOR COMFORTABLE POSITIONS
At the beginning, you may think no comfortable position exists. Here is where the need for patience comes in. When we are in pain, we tend to look for a quick fix, so we try to find a comfortable position but if we don’t succeed or only do so partially, we get discouraged and abandon the search. Some positions actually are better than others and “getting a little better” is the first and crucial step.
I remember a patient I will call Peter who came to my office in such excruciating pain that he could not tolerate any position for more than two or three minutes. We spent the entire 45-minute session searching for postures in which his pain would be at least tolerable. Gradually, over a period of a few sessions, Peter was able to tolerate longer periods in one position. Eventually, after a few months, Peter became pain free, even though his MRI showed a ruptured disc compressing the nerve roots.
Here are a number of positions that many back-pain sufferers have found helpful:
A. Side lying with pillows between your thighs, knees and lower legs.

B. Hook lying—on your back with lower legs resting on a chair, bed or sofa
This is especially helpful when you find that lying on your back with your legs straight increases the intensity of the pain but having your knees bent helps reduce the pain!

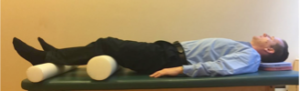
C. A version of the above-described position can be achieved by using rollers (rolled beach towels or pillows) under the knees.
D. Kneeling and resting your torso (including abdomen) on a bed, ottoman or sofa
E. Lying on your stomach
Some people find this position very helpful, although for many it could be impossible. Here again there are many variations. Try it, for example, with a pillow under your belly or your hips and your head turned toward one side.

Another version of the prone position is achieved by lying on the stomach with the head turned, the knee on that side pulled toward your chest and the elbow (on the side of the bent knee) bent with the hand near your face. The opposite arm is down along the side of the body.


Those for whom arching of the back brings comfort may prefer to lie on the stomach with elbows bent, sometimes even leaning on the elbows, forearms and hands (sphinx position). Remain in this position for 20-30 seconds and observe if it brings you some relief.

The important thing is to find on your own which of these positions gives you the most comfort. This brings us to the next point.
5. CHANGE POSITIONS FREQUENTLY
Staying in one position for a long time (even a comfortable one) contributes to stiffness, weakness and more pain. During waking hours try to change position every 15 to 20 minutes. Sit a little, lie down a little and walk around a little, even if it is just a short stroll to the bathroom or the kitchen for a glass of water. Proper movement, within your range of comfort, will help you to limber up, reduce muscle spasm and release muscle tension. Avoid bed rest! Rest should only be used for severe pain and then only for one to two days.
Did you know:
- For every two days of bed rest, heart rate increases one beat
- In healthy men, the rate of bone loss increases 50 times with bed rest. Although bone minerals are gradually restored after bed rest, the rate of restoration is four times slower than the rate of loss.
- For every week of complete bed rest, muscle strength declines 10 to 15 percent. Muscles lose their elasticity and joints lose their full range of motion when they are immobilized for extended periods of time. That’s why it’s hard to get your legs moving again after hours sitting in a movie theater.
6. PROLONGED SITTING SHOULD BE AVOIDED
If your pain increases with sitting, minimize the amount of time you spend sitting. It has been documented that maximum pressure on the damaged discs can occur in sitting positions, especially when coupled with a slouched, bent-forward posture. Sitting on soft couches and sofas may be especially problematic as they may cause you to lean on your sacrum and tailbone, tilt your pelvis backward and bend your lumbar spine. There are two actions that may help you improve your sitting posture:
A. Discover your sitting bones.
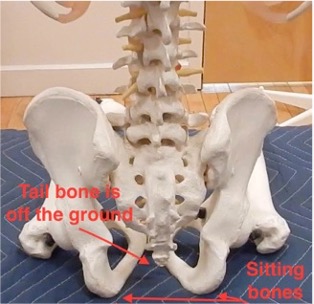
Your ‘sitting bones’ (technically called your ischial tuberosities) are designed for effective weight bearing in sitting.
To identify your sitting bones while sitting upright, place your right hand under your right buttock and shift your weight forward and backward, and from side to side. You should be able to feel the hard, round shape of your sitting bone.
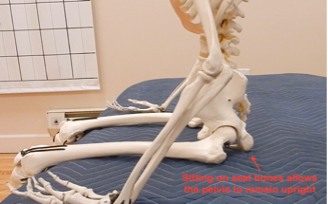
Repeat the same process on the left side. Sitting on the forward edge of a chair will help you to identify these important bones. Notice how upright your pelvis and spine become when you sit directly on your sitting bones. This is the safest and most efficient way of sitting – your skeleton can remain upright without strain, contraction or muscular fatigue. In fact, a skeleton can sit by itself – see the photo below!
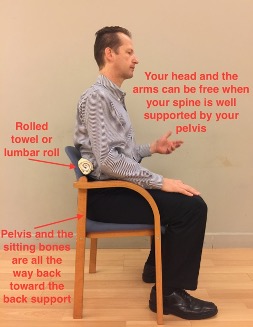

B. Use lumbar supports
A rolled towel or a lumbar roller will help you keep your pelvis upright, preserving the natural curve of your spine, and helping you to keep your lower back straight. Also, during the acute stage of lower back pain, avoid sitting in positions where your knees are higher than your hips (such position may cause excessive rounding of your back).
7. DO A LOT OF DIAPHRAGMATIC (BELLY) BREATHING THROUGHOUT THE DAY
Belly breathing is a great way to reduce tension, pain, physical and emotional stress. Many systems such as yoga, meditation, relaxation training and biofeedback use this type of breathing. A correlation between poor function of the diaphragm and chronic low back pain has been documented in recent studies (“Postural Function of the Diaphragm in Persons with and without Chronic Low Back Pain”, Journal of Orthopedic Sports Physical Therapy, 2012.)
Here is how to do it:
- Assume a position that is most comfortable for you. This can be done in any position. Place your hands, or at least one hand, on your lower abdomen so you can monitor the movements; your hands are below your belly button and above the pubic bone.
- As you inhale, your abdomen expands in all directions, like a balloon. When you exhale, simply allow your belly to sink down without any effort. If possible, inhale through your nose (it filters and warms up the air) and exhale either through your mouth or nose. As you exhale, focus on releasing tension and letting go.

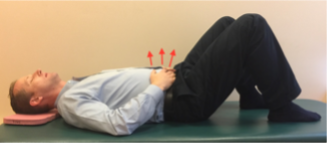
- Make it simple, even if at the beginning you find your breathing is short and shallow or that you tend to hold your breath. Do not try to improve by forcing your breath. Do not try to correct anything. Just simply breathe in and out, be fully present and bring your awareness to every breath and you will find that within just two or three minutes your breathing will improve spontaneously.
Recently I worked with a patient I’ll call Jane, who experienced a very sharp pain, especially as she changed positions. During the first session, she was in so much pain she could not stand upright. She was bent over and her chest was shifted to the right. Here is how we applied belly breathing to lessen her pain: Jane would take five slow diaphragmatic breaths before getting up from the bed. As she sat up, her pain became severe, so she took another five breaths in the sitting position. Then she stood up—and took another five breaths. Jane would walk 10 or 15 feet, then get back into bed and take another five breaths. She practiced this diligently many times throughout the day. In two days, her pain was significantly lessened, and she was able to stand and walk upright.
8. ROLL TO GET OUT OF BED
Often getting in and out of bed is accompanied by severe pain. One way to reduce the pain is to limit spinal movements. I do not recommend fixing or holding the spine motionless in the long run, but during the acute stage it can be very helpful. Imagine you are wearing a brace or corset that keeps your pelvis and your ribs in a fixed relationship (that is, your torso is just like a cylinder). It may take some practice before you master this technique.
Now, from a laying down position on your back, with your knees bent and your feet a shoulder-width apart, roll onto your side. Your knees, pelvis, chest, shoulders and head should roll like one unit to prevent twisting. Then, from this side-lying position (close to the edge of the bed), let your lower legs swing off the side of the bed while you push with the upper hand and the bottom elbow. Your body, again, is held like one unit. The weight of your legs will help lift your head and upper body into the sitting position.
Photo Sequence of Transferring from Lying to Sitting







9. GETTING UP FROM A CHAIR WITH A “LONG SPINE”
You don’t need to bend, arch or twist your spine to get out of a chair. The following three strategies are similar to the one described for getting out of bed and focus on keeping your spine long, minimizing strain on your lumbar region:
A. Using one or both arms to push off a back of a chair or armrest. Try putting one foot under the chair (actually under your pelvis) to avoid unnecessary movements of your spine.

B. Standing up with a spiral turn can help you to maintain the integrity of your spine. In order to perform it successfully, make a swiveling movement with your legs, pelvis and the entire torso until one of the buttocks slides off the seat. Your foot needs to be well under the side of the pelvis for proper balance. As you swivel, your heel will automatically lift preparing the ball of the foot and the toes to push your body upward. Continue straightening your knees while maintaining the uprightness of your spine. You will end up standing sideways to the sitting surface. It may be easier for you to do this towards one side than the other.




C. Eventually you will be able to get up from a chair without using your hands, moving straight forward and up. Please sit on the front edge of the chair. Lean your trunk forward by moving in your hips. Your pelvis will tilt forward, but the lumbar spine should remain unchanged! Imagine that you have a scotch tape glued to your back along the sides of your spine – do not rip the tape off as you lean forward.
Photo Sequence of Standing Straight Forward and Up
1. First practice just the beginning of the movement. Do these simple movements back-and-forth until you can perform them without any increase of pain.

2. Gradually increase the size of the movement until you are able to lift your buttocks off the seat of the chair.

3. Think of leaning forward instead of getting up from the chair. You may surprise yourself by getting up with barely any effort. Search for the path that is easiest and most pain-free for you.


10. STRATEGIES FOR GETTING DRESSED
Usually, when one has back pain, the most challenging part of getting dressed is putting on the socks and shoes. You may want to try the following option:
A. Lie on your back with knees bent. Bring one foot up toward your chest, opening the knee out to the side; cross one ankle over the other (bent) knee, thus allowing your hands access to your foot.

B. You can use a similar movement sitting on the edge of a chair or bed. If it is too difficult to cross your legs, you can try to sit farther back on the seat and place your foot on the bed with your knee bent to the side or you can place another chair in front of you and rest your foot there. Avoid rounding of your back.

One of the secrets to a healthy and pain-free back is learning to move and act with a sense of lengthening of your spine. Becoming more aware of the distance between your head and the pelvis during everyday activities may be instrumental for your recovery and help to prevent future difficulties.
Tying your shoes may be a challenging activity, not only during the initial phases of acute back pain, but in general. Shortness and compression of the spine when bending forward is a common culprit.
Let’s take a look at the two photos below. The first picture is how NOT TO BEND FORWARD. Please note the excessive rounding of the back. The pelvis is almost vertical while the upper trunk is leaning forward! This exposes the lower lumbar vertebra and the intervertebral discs to a tremendous strain. In addition, please notice how short is the distance between the head and pelvis. Such shortness creates a compression and strain in the lower lumbar region. The second picture illustrates a better movement strategy for tying shoes. There is more movement in the hip joints allowing the pelvis to tilt forward and making more uniform and harmonious bending of the entire spine.


11. PRACTICE RELAXATION AND LIMBERING EXERCISES
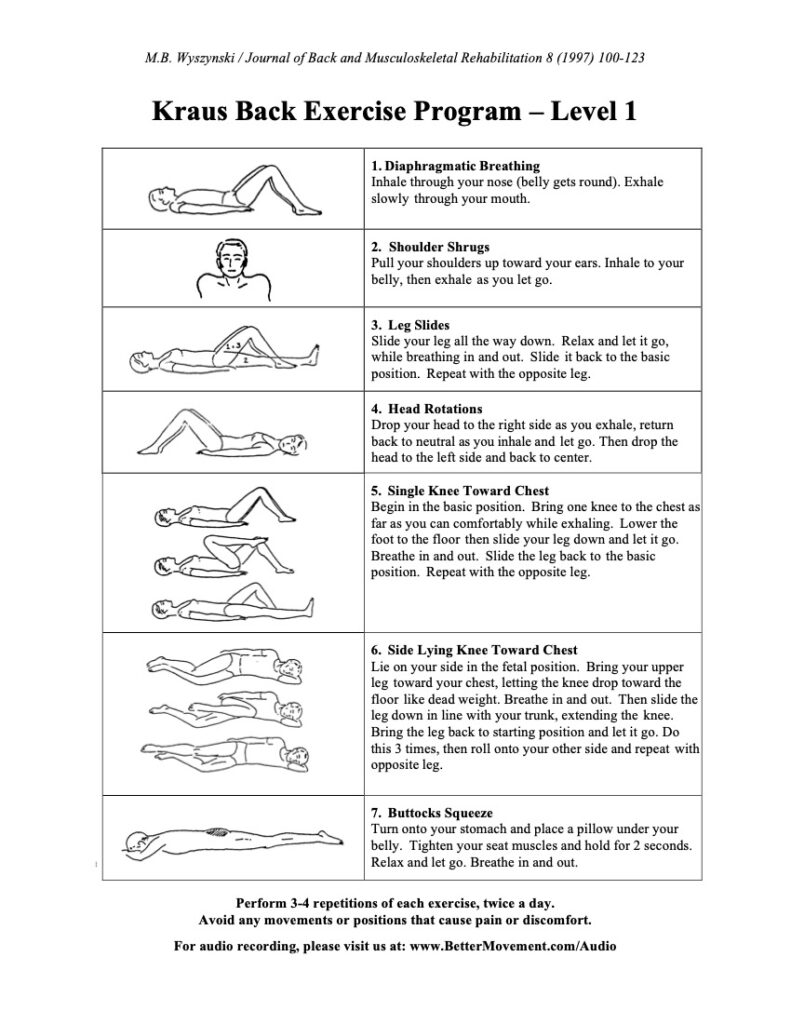
Dr. Hans Kraus, with whom I had the privilege of working, designed a simple, yet effective, set of back exercises. His idea was to create a universal program that would be safe and helpful for most back pain sufferers. A study involving 11,809 subjects showed that 80% of participants using these exercises reported pain reduction in six weeks.
The first seven out of Dr. Kraus’s 21 exercises I find particularly helpful in the early stages of recovery from acute back pain. See the attached illustration of the first level of the back exercise program.
I recommend you review these exercises with a medical professional (preferably a physician or physical therapist) to make sure they are suitable for you. Please use these exercises responsibly. Stop if you feel any increase in your symptoms. You should feel better after performing the relaxation and limbering exercises.
It is possible that you need to start with only the first three or four and not the entire seven movements. The emphasis should be on letting go; relaxation at this point is much more important than stretching. All the movements should feel simple, easy and pleasant.
Three or four repetitions of each exercise are sufficient. The idea is to move a group of muscles and then let them relax as you work on another group. I usually recommend two exercise sessions a day (morning and evening). Do not rush through them. It should take about 12 to 15 minutes to do the first seven exercises.
12. CONSULT WITH A FELDENKRAIS PRACTITIONER
The Feldenkrais Method can be extremely useful in the treatment of acute and chronic back pain. There are a number of reasons why I find this approach to be so beneficial:
- Feldenkrais treatments are gentle and safe. It is essential -especially during acute episodes of pain- to avoid additional strain and to avoid flare-ups or setbacks.
- Feldenkrais practitioners are trained to pay attention to subtle nuances in your postural organization and habitual movement patterns. These small details often make a big difference in the alignment and movements of your spine, and can influence your process of healing.
- Feldenkrais exercises and treatments are designed to help you learn how to use your entire skeleton when you move. This is important because most of us in general don’t think much about movement, take it for granted or actually don’t believe that our movement habits can be changed.
It is well understood and accepted that pain can alter posture and movement through substitutions, compensations or avoidance. What is less apparent, however, is that an inefficient movement itself is enough to cause pathology and pain.
For example, it is obvious that disc herniation can cause postural shifts, misalignment, and difficulties with movement of the spine but the reverse is also true: the herniation of intervertebral disc can be a result of months or years of overuse through excessive movement and accumulation of compressive and shearing forces. The Feldenkrais method can help you move better, reducing strain on your muscles, tendons, ligaments, discs and joints.
- Recalibrating the balance of your sympathetic and parasympathetic nervous system is of the utmost importance. I find most people who are in pain exhibit symptoms of sympathetic system dominance, characterized by the “fight or flight” state and constrained breathing, and elevated heartbeat and blood pressure. This causes a heightened contraction of the muscles that serve to brace and splint the injured areas. On one hand, this is a wonderful survival mechanism, which helps us to prevent loading or moving a broken bone, torn muscle or ligament, or injured disc. This natural reaction to injury is essential for survival immediately following the injury.
However, this accommodation can linger and become habitual and detrimental. Most of our tissues heal within the first six weeks after an injury. In order to recuperate, our organism needs to return to a healthy, parasympathetic state.
This will promote the conditions necessary for healing, including healthy breathing and the gradual restoration of free and easy movements. The relaxation of tense muscles will facilitate improved blood and lymph flow to the injured areas, which is crucial for the healing process to occur. Feldenkrais lessons can be extremely helpful in facilitating your return to a healthy parasympathetic state.
- Feldenkrais helps to break the vicious cycle of pain and can help you to regain confidence in your own body. It also helps to prevent the pain from becoming a learned behavior that is ingrained in your brain.
I recommend that you work with a Feldenkrais practitioner who has experience helping people with low back pain and sciatica.
13. USE HEAT AND COLD
There is no rigid rule about applying either heat or cold. Try to find out for yourself which works better for you. Sometimes alternating both heat and cold packs may be more beneficial. Be aware that people with diminished skin sensitivity (especially diabetics) should be very careful in the use of topical heat or cold packs.
A. Cold packs are usually most effective right after the onset of the pain/injury. Ice packs help to relieve muscle spasm, reduce swelling and inflammation.
Wrap the cold pack in a towel and check your skin frequently to prevent frostbite. Eight minutes, two or three times a day, is usually sufficient but you may repeat cold pack applications as often as once an hour.
B. Hot packs are effective in releasing muscle tension and improving blood circulation, which are essential for healing. Moist heat is preferable because it penetrates better than dry heat. Most hot packs for home use these days are microwaveable.
Use the hot pack for 15 to 20 minutes at a time, two or three times a day. A good alternative is “Thermacare” which is available in most drug stores. It is self-adhesive, so it can be worn for up to eight hours, allowing you to benefit from heat therapy while moving around freely.
14. ACCEPT THE FACT THAT HEALING TAKES TIME
For some people relief from pain may come in just a day or two; others may need a week or longer. With back pain, as with other ailments (like the flu, for example), you cannot rush things. A sense of urgency creates additional stress, which can actually make things worse. You become tense and irritated, thus making your muscles more prone to spasm and slowing your progress. Getting upset brings no benefit. Just as with a common cold, you need a few days to get better.
The proper conditions for healing can markedly speed up the process of recovery. When you have the flu, you stay in bed, drink lots of fluids and take medication to create the proper conditions for recovery and to prevent complications like pneumonia. The same applies to back pain.
Your office will survive a few days without you. The “urgent” projects can wait or be done by someone else. In a nutshell, right now your system needs to be taken care of. The good news is that you can change and your condition can improve. But don’t set any deadlines. Accept the fact that healing takes some time.
15. A FEW WORDS ABOUT CLOTHING
During the time of recovery, you should ideally wear loose, comfortable clothing that allows you to breathe and move freely.
Avoid tight, low-cut pants that tilt your pelvis backward while sitting. Some low-waistline trousers make it practically impossible to maintain a correct sitting position! Also, avoid putting your wallet, keys, and cell phone in your back pockets. They may cause an asymmetrical position of your pelvis and spine, and also cause pressure and irritate muscles and other soft tissues in your buttock area. The same applies to tight belts that can compress the sacrum, pelvis and the lower back area.
Wear only comfortable shoes. In general, avoid high heels and platform shoes as they displace your center of gravity and challenge your balance. Make sure sandals have a strap behind your heel and that you wear the right shoes of the right size – shoes that are too loose may cause excessive gripping with your toes and result in unnecessary tension. Your feet need to be powerful and relaxed.
16. LIFESTYLE CHANGES
Sometimes our habits and lifestyle choices play a role in our comfort and our ability to heal from back pain. If you experience back pain frequently, you may wish to consider the following:
Research has indicated a possible link between smoking and low back pain. Smoking, hypertension and coronary artery disease – all of which are risk factors for atherosclerosis- have been associated with the development of low back pain. At the annual meeting of the American Association of Orthopedic Surgeons in San Francisco, in 2001, presenters demonstrated evidence that one cause of injury and low back pain may be damage to the vascular structures (occlusion of the arteries) that supply the discs and joints.
Similarly, high levels of cholesterol were significantly associated with the development of degeneration of the spine (spondylosis). And, a number of studies showed a strong correlation between low back pain and increased body mass index (BMI). So, you may wish to try shedding a few extra pounds. Losing weight may help you to reduce and recover from back pain, and also improve your energy and breathing.
Although alcohol is a muscle relaxant, while recovering from back pain, you should avoid drinking alcohol as it may interact negatively with medication. For example, alcohol can cause liver problems when combined with acetaminophen (Tylenol), and stomach ulcers and bleeding when combined with aspirin or non-steroidal anti-inflammatory medication (NSAIDs). The interaction of alcohol with antidepressants and narcotics can be fatal. In addition, consuming alcohol may alter your movements and judgment. A few drinks can numb the pain temporarily but also put you at risk for making potentially injurious movements, which may exacerbate your back problems.
17. USE YOUR IMAGINATION
The use of imagination can produce immediate, positive results. When my own back “went out,” I remember sitting on my bed getting ready to stand up, expecting to experience the pain I had felt every time I tried to get up.
On my first attempt to stand, I experienced a sharp back pain. Instead of fighting it, I sat back and tried to imagine what I would have to do if I wanted to jump forward and perform a forward roll. Of course, this was an outrageous idea. I could barely move! Still, I allowed myself to imagine the process.
I asked myself how my feet would have to be placed to allow such a movement—and adjusted them to fit the image. Then I considered how I would have to sit on the bed. Would my pelvis be forward or back? With each attempt, I found something in my body’s organization that I could simply adjust or change. The whole process of imagining these positions took about two minutes. Then I swiftly got up without any pain. It was a revelation!
One of the functions of our brain is to solve problems. We must give it a chance to work. A number of research studies show that the mind itself, merely by thinking, can change the brain. In one experiment, two groups of volunteers played a five-finger piano exercise.
One group practiced on a piano; the other group merely thought about practicing it. While actual physical practice produced changes in each volunteer’s motor cortex, so did mere mental rehearsal. Like actual movement, imagined movements change the cortex. (Schwartz and Begley, The Mind and the Brain: Neuroplasticity and the Power of Mental Force, Regan books, 2002.)
If you want to improve an action using your imagination, choose an action that is familiar to you, and make it much more challenging. You need a clear picture of the action in your mind. If you have never done a somersault, don’t use that as an image because it would only be an abstract concept for you. You need to select a concrete sensory experience, something challenging but familiar.
For example, if you want to improve your ability to push open a heavy door, try to imagine how you would organize your body to push a car or a heavy piece of furniture. If lifting a teapot is a problem for you, imagine how you would use your body to lift a heavy suitcase.
Try it. You may have an “Aha!” experience.
CONCLUSION:
I hope the practical information outlined in this article helps you cope with the acute back pain and will inspire you to take good care of yourself. Perhaps you have been tense, under emotional and physical stress or overworked. Maybe you did not get enough sleep, your diet was far from ideal and/or you did not have enough time for proper exercises and rest.
Sometimes pain can be a great motivator to make the necessary changes in our lifestyles. The Dalai Lama said: “The goal is not to be better than other men, but your previous self.”
Please keep this article as a handy reference and feel free to share it with others.
REFERRED EXERCISES FOR RELAXATION AND LIMBERING – SECTION 11
The must-have program Marek has used successfully with thousands of clients for over 30 years to treat acute back pain or flare-ups.
This on-demand online format for self-care includes a 13-minute daily exercise program to perform twice a day, 7 lessons to help you understand and master the daily exercises, and essential guidance on how to cope with back pain.